We do palliative care, at your place or ours
We do palliative care, at your place or ours
Jump to section:
Facing a life-limiting illness is complicated
But at HammondCare, we do complicated.
Our multidisciplinary palliative care services are there to help you or your loved one live as well as possible.
While palliative support is embedded in our all of our residential and home care services, in all our areas, we are able to offer specialist palliative care in parts of Sydney, at your place or ours.
Wherever you are on your journey, our skilled, compassionate specialists and carers can support you to handle whatever comes, in a way that works for you and your loved ones.
TimPascoePhoto0451.jpg?width=1772&height=1182&name=HC06-07-04-24(C)TimPascoePhoto0451.jpg)
It's all about you
Our specialist palliative services bring you leading clinical expertise, world-class research and a compassionate approach to care.
Care tailored to your unique needs
Every person deserves to be heard and have their unique needs met. That’s why we get to know you and create a personalised care plan that’s right for you.
Your dedicated specialist team
You will be cared for by a consistent team of multidisciplinary specialists who work with you and your family to provide the highest quality care.
Research informs all aspects of care
As leaders in world-class palliative care, we continually innovate care delivery and education using the latest research from The Palliative Centre.
Explore researchA variety of locations to suit you
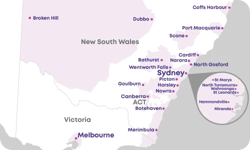
Whether you’re in need of our inpatient unit or community palliative care, you’ll find a choice of convenient locations in northern and southwest Sydney.
Browse locationsWhat support is available?
It's your choice
You can choose from a range of programs to support you in hospital or at home with expert, wholistic care.
There is no cost to use our palliative and supportive care because we’re subsidised by State Government funding.
And if you choose to use your private health insurance, you won’t be out of pocket.
In hospital
When you are admitted to the palliative care unit, a team of specialists from diverse disciplines - medical specialists, palliative care nurses, physiotherapists, speech therapists, social workers, occupational therapists, dietitians and pastoral care - comes together to provide compassionate support and holistic care.
This multidisciplinary team works together to keep you as well and as comfortable as possible.
You can be admitted:
- for a short period to help manage symptoms of a life-limiting illness, like pain
- to meet your needs and those of your family and carers in the final stages of your journey
At home
Our community palliative care and outpatient clinics can tend to your needs where you’re most comfortable – in your own home.
We offer:
- pain relief and management of symptoms
- 24/7 specialist palliative care expertise
- phone support
Private health partnerships
We've partnered with Medibank and Bupa in the Northern Sydney Local Health District to make palliative care services available to you at home, so you can live as comfortably as possible, for as long as possible.
Our partnerships give you
- The option to stay in your own home, with specialist palliative care nursing support
- Around the clock phone line
- Weekend visits from palliative care nurses
- Emotional, social and spiritual support
- Ongoing assessment and support
Want to know more? Give our friendly team a call.
How to access palliative and supportive care
There are three steps to getting a referral for our palliative and supportive care services.
Referral
Assessment
Care Plan
Tell us what's going on
Get in touch to find out more about palliative care or referrals.
Online support
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt.
Online support
Important information about referrals
When you ask your GP or specialist for a referral, it must include:
- the referring practitioner’s address
- phone number
- provider number.
If the referral is from a specialist, your GP’s details should also be included with the referral. All referrals must be legally valid as outlined in the Medicare Benefits Schedule (MBS).
Please ensure the letter of referral is addressed to our team. The referral must be received and dated before treatment can start.

Refer a patient for care
Visit our Healthcare Referrals page to learn more about the palliative referrals process.
Find our palliative care
Our specialist palliative care services are available in northern and south western Sydney.
Bereavement support
Bereavement counselling is a confidential discussion with a trained professional when you’re experiencing grief. They will help explore the impact of your loss and identify coping strategies. Grief and bereavement are different for everyone, and seeking help early supports continued healing.

Learn about the end of life
Many of us caring at home can feel unsure about our role as the end approaches.
The Last Days Program helps you understand what to expect during the dying process and death.
Developed in consultation with carers to increase knowledge and confidence at this difficult time of life, the program gives practical advice about topics we sometimes find hard to discuss.
For more on how to support your dying loved one,
download our brochure or visit our Last Days information page.

The latest in quality end-of-life care

2 December 2024 | Article
What exactly is palliative care? It might not mean what you think

25 May 2022 | Article
The Advance Project boosts confidence for sensitive conversations about end-of-life

2 December 2022 | Article
Resources about grief or end of life care
More resources to support your family
We’re here to talk. Call us now.
If you need some guidance on what to do next, our team can help. Call 1800 998 111 or send a message.