Our position statements
Our position statements
Our views on issues that matter
Voluntary assisted dying
Our view
Under laws enacted now in all states of Australia, voluntary assisted dying (VAD) enables an eligible person to ask for medical assistance to help end their life because they are in the late stages of an advanced disease or illness, and feel they have ‘intolerable suffering’. We consider every person – to the very last day of their life – to be precious. They should have access to appropriate palliative care regardless of location or circumstance, so improved access and funding remain urgent priorities.
We recognise that VAD is a process, not a specific act, and that we may be caring for patients, residents, or clients at any time in this process.
We have put in place careful protocols and processes in relation to requests for VAD, and our team are trained in how to respond and will always do so with empathy and respect.
Our number one priority remains the people we care for and their well-being, with the provision of quality palliative care in a compassionate context our goal.
Approach
Because of these views, we have developed the following principles in relation to VAD:
- Human life is of intrinsic value - we support equal access to quality palliative care for all people with serious life limiting illnesses.
- We don't support VAD, including physician-assisted suicide, nor do we recognise these interventions as medical treatments.
- We'll always respond with compassion and care for residents, clients, and patients and respect their right to choose.
- We won't facilitate or participate in the delivery and/or management of the act of VAD but will continue to provide all other care for every resident, client and patient.
- Residents, clients or patients in our care who choose to make use of this law will not be impeded in any way.
- We'll always support our team and their protected right to conscientiously object to participating in the voluntary assisted dying process.
- Our focus will remain on quality palliative care.
Learn about our Palliative and end-of-life care
Design principles
Our view
HammondCare has a long history of researching, refining and delivering world class specialist dementia design principles and innovation. In partnership with in-house expert care practitioners, the HammondCare Design Team pioneered the cottage model in 1995, with continued refinement since then.
Approach
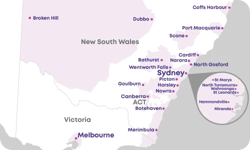
Accommodating between 8 to 15 residents each, HammondCare has built more than 65 cottages across NSW, Victoria, and South Australia aligned to these principles:
- maximise independence
- compensate for disability
- enable staff to provide care
- enhance self esteem and confidence
- manage unwated stimuli
- welcome relatives and integrate with the local community
- be orientating/legible
- reinforce personal identity.
This design model is based on and well-supported by research. The INSPIRED Study[1] from Flinders University that in the cottage model, residents were:
- 68 per cent less likely to be hospitalised
- 73 per cent less likely to have an emergency department visit
- 52 per cent less likely to be exposed to potentially inappropriate medications
Advocacy
The cottage model (also referred to as the household model, or clustered domestic residential aged care) is considered best practice, especially for those living with dementia. The Royal Commission into Aged Care and Quality Standards in 2021 stated: ‘good design in residential aged care, particularly for people living with dementia, usually involved smaller, lower-density congregate living arrangements rather than larger, more institutional settings.’[2]
In response to the Royal Commission, HammondCare welcomes the four principles outlined in the Australian Government’s draft National Aged Care Design Principles and Guidelines, to be finalised in June 2024. We believe it is feasible for elements of these design principles to be implemented by providers within existing buildings and to use the principles when renovating or constructing sites:
- enable the person
- cultivate a home
- access the outdoors
- connect with the community.
HammondCare’s eight design principles encompass those in the Government’s draft guidelines and are the foundation of design at HammondCare (see graphic). They provide an overarching framework of good design for older people and people with dementia. These principles are followed when planning a new build or refurbishment project. Their implementation is clearly seen in the earliest cottages and the most recent, while incorporating learning and improvement in how the principles continue to be implemented.

[1] The Medical Journal of Australia 2018, ‘Clustered domestic residential aged care in Australia: fewer hospitalisations and better quality of life.’
[2] Commonwealth of Australia 2020, ‘A Summary of the Final Report’, Royal Commission into Aged Care Quality and Safety, p. 105.
End-of-life care
Our view
HammondCare considers life to be intrinsically valuable[1] and supports equity of access to quality palliative care for all people with life limiting illnesses.
Advocacy
HammondCare is particularly focused on advocating for more funding and resources to improve education, research, and service delivery of dementia specific palliative care. Dementia is the second leading cause of death for people in Australia.[2] Despite this, there is a lack of dementia-specific palliative care services and people with dementia are less likely to receive palliative care[3]. With in-house expertise and 30 years’ experience in dementia care, HammondCare is uniquely placed to strengthen integration and the delivery of palliative care for people with complex dementia, through shared expertise, relevant frameworks, assessment tools and best practice service delivery.[4]
More broadly, issues preventing access to palliative care include:
- unequal service provision, which particularly impacts communities living in regional and remote locations and under-serviced metropolitan areas[5]
- chronic under-funding that is fragmented between different levels of government
- staff shortages
- lack of community awareness.
Research has shown that most people express a preference to receive end-of-life care in their home, yet palliative care remains difficult to access outside of hospital settings.[6] HammondCare aims to develop models, advocate for policy changes and funding models that deliver better palliative care in homes and in residential aged care. There is a particular funding and care gap when residents become palliative during their time under the Australian National Aged Care Classification (AN-ACC) funding model. HammondCare proposes the provision of a lumpsum payment on entry to residential care that represents the average care and funding costs associated for a person when they enter palliative care.
HammondCare does not recognise voluntary assisted dying (VAD) as a medical treatment and will instead champion access to palliative care, while always responding with compassion, respect and care for residents, clients and patients, in compliance with legislation. HammondCare believes it is vital to improve access and availability to palliative care and avoid it being withdrawn or reduced within the context of VAD, now that it has been legalised in all Australian states.
[1] Psalm 139:13-16 & Genesis 1:26-27
[2] AHIW (2022). Dementia in Australia Summary Report
[3] Dementia Australia/Palliative Care Australia (2017). Palliative Care and Dementia, p. 9.
[4] HammondCare Research Arm (2022). Facilitated case conferences on end-of-life care for persons with advanced dementia – a qualitative study of interactions between long-term care clinicians and family members
[5] Australian Government Department of Health (2019). Exploratory Analysis of Barriers to Palliative Care Summary Policy Paper
[6] Grattan Institute (2014). Dying Well report
Environmental stewardship
Our view
HammondCare’s Mission in Action compels us to be good stewards of God’s creation. Promoting sustainability aligns with our identity as an independent Christian charity. To achieve this, HammondCare is committed to reducing our environmental impact and promoting sustainable practices across our operations. We recognise the importance of environmental sustainability for the wellbeing of residents, patients, clients, our people and the broader community, and are committed to taking action to create a more sustainable future.[1]
Approach
We prioritise four areas of sustainability:
- Energy efficiency: Reducing our contribution to climate change and dependence on fossil fuels through effective energy management practices.
- Waste reduction: Implementing best practice waste management systems and reducing the amount of waste sent to landfill.
- Sustainable design: New developments have comprehensive sustainability plans and targets that take a holistic approach to minimise environmental impact.
- Sustainable travel: Traveling in environmentally responsible and efficient ways, reducing our carbon footprint and promoting sustainable transportation practices.
In line with these priorities, we regularly update our sustainability strategy which covers the key areas of water and electricity use, solar generation, waste reduction, fuel consumption and the use of smart technologies for managing resource use.
HammondCare’s mission is to improve quality of life for people in need. We recognise there are sometimes tensions between delivering high-quality care while optimising sustainable practices. The sustainability initiatives we undertake will always align with our integrated Philosophy of Care and best practice Design Principles.
We acknowledge that our common use of single-story care homes, dependency upon single-use personal protective equipment and incontinence products contribute to built-in inefficiencies. Within this context, we strive to do more than the minimum standards for sustainability, complying with state and federal legislation.[2]
[1] Environmental Management. Environmental Stewardship: A conceptual Review and Analytical Framework (2018).
[2] NSW Government (2022). Comply with NSW environmental legislation.
Australian Parliament House. Chapter 2: Environmental regulation in Australia.
Learn MoreHomelessness in aged care
Our view
HammondCare’s charitable journey began with provision of rent-purchase homes for more than 110 families experiencing homelessness during and following the Great Depression. This focus continued with the provision of homes for aged ‘battlers’ during the 1950s and continues to be an urgent priority today. As part of our organisational DNA we have never lost this commitment to support people experiencing or art risk of homelessness. We have been at the forefront of innovative approaches for providing homes and support to those who need them most.
Now in the 21st century, HammondCare is particularly committed to supporting older people with a homelessness experience by providing long-term stable homes with high level complex care. HammondCare places a strong emphasis on relationship-based care for people experiencing or at risk of homelessness. Our Philosophy of Care underscores the significance of supporting the social, health and legal aspects of an individual’s wellbeing. When addressing homelessness, our approach prioritises:
- intelligent and measured risk management
- trauma-informed care
- development of security and trust.
Advocacy
Our key position on addressing the needs of older people experiencing or at risk of homelessness, is that it requires enhanced and streamlined funding from both state and federal governments, as well as trusts, foundations and philanthropic organisations.
An example of what can be achieved is HammondCare Darlinghurst. Opened in 2020, it is an innovative, purpose designed, residential care home with 42 private rooms for older people who were experiencing or at risk of homelessness. The construction of this care home could not have been achieved without support from local government and donors.
The combination of small household design (in a multistorey apartment-style building), trauma-informed, relationship-based care and strong community connection has produced positive outcomes for the most vulnerable. Research shows a marked increase in self-reported wellbeing, reduced severity of mental health symptoms, and maintenance of physical functional ability in daily living tasks with no decline in objective cognitive ability. HammondCare plans to expand its older people’s homelessness residential aged care services and serve the growing need in inner Sydney.
HammondCare is ready to expand its care offering for older people experiencing or at risk of homelessness but has found it difficult to proceed from a site selection and capital funding perspective.This is despite knowing the approach at Darlinghurst results in an average annual government saving of $32,000 per bed when comparing 12 months pre and post admission cost-utility data, without any decline in resident-reported quality of life.[1]
Further, our experience shows that regular aged care approaches are not well equipped to support people experiencing or at risk of homelessness, while general homelessness services struggle to support the needs of older people.
This represents a significant and growing gap in care provision for increasing number of vulnerable older people with insecure housing and complex care needs.
[1] HammondCare (2022). HammondCare Darlinghurst – caring for those who others can’t or won’t.
Homelessness servicesManaging safety with dignity
Our view
HammondCare promotes safety and the dignity of choice through relationship-focused care and environmental design in residential care. This includes a risk management, rather than a risk avoidance, approach.
Approach
Our relationship-based care puts the person first, ensuring safe practice and risk management is balanced with resident choice and independence:
- Our relationship-focused staffing model helps teams to get to know residents – each cottage has a dedicated multidisciplinary team, prioritising continuity of care. Each resident has an assigned Care Manager who develops a trusting relationship and understands each resident’s personality, preferences and needs through close daily interactions. Care teams are empowered to use compassionate and creative strategies to meet resident needs and prevent distress escalating.
- Our case management approach tailors care with residents and their families and carers at the heart of decision-making. Empowered care teams develop individualised care approaches to meet needs, preferences and goals. Throughout life, individuals display different levels of risk appetite which is also taken into account. For residents living with dementia, behaviours impacting on care are investigated to find any underlying causes (e.g. pain, carer approach) and addressed creatively and with compassion. Restrictive practices are always a last resort, following a thorough assessment and all other psychosocial interventions have been exhausted, in line with regulatory requirements.
Advocacy
HammondCare supports built environments that facilitate safety without restriction. HammondCare’s evidence-based design principles are exemplified in its cottage-style household model which is recognised as best practice. Cottage-style aged care accommodation was pioneered by HammondCare nearly 30 years ago and continues to be endorsed as best practice. For example, the Department of Health and Aged Care’s new draft National Aged Care Design Principles and Guidelines align with our long-standing design principles. As well, the Royal Commission into Aged Care Quality and Safety endorsed the cottage model in Recommendations 45, 46 and 142 of its final report.[1] The model facilitates safety without restrictions, by:
- Enabling independence – good visual access and clear lines of sight assist residents to navigate freely and independently.
- Promoting agency – clear pathways throughout the home and between indoor and outdoor areas allow residents to freely access all areas.
- Maintaining a home-like environment – shared spaces like kitchens and dining areas are central in the home and intentionally accessible at any time. Staff-specific areas are kept behind hidden doors to prevent resident confusion and access attempts.
HammondCare does not use video surveillance. In addition to our built environment and relationship-focused care management approach, HammondCare uses proactive strategies to maximise safety, including the use of unobtrusive technologies (e.g. passive infrared sensors), and a reporting culture where our people are encouraged to identify and respond to risk.
[1] Royal Commission into Aged Care Quality and Safety, Final Report Volume 1, https://agedcare.royalcommission.gov.au/sites/default/files/2021-03/final-report-recommendations.pdf
Residential CareModern slavery
Many people may be surprised to learn that Modern Slavery is a real and important issue that requires focus in Australian communities and workplaces.
HammondCare rejects any form of modern slavery and is committed to ensuring our operations and policies are aligned with identifying and managing modern slavery risks.
Read Our StatementReconciliation Action Plan
We acknowledge the valuable contribution of First Nations people to whom we’ll listen as we learn, building our understanding of history and culture. It is only by taking these first steps that we can deliver care that is culturally safe, inclusive and informed.
Find out more
Spiritual and pastoral care
Our view
Central to HammondCare’s motivation are the Christian principles and values expressed in the words and deeds of Jesus. HammondCare believes in the value of all people as made in the image of God and loved by God. This compels us to go above and beyond for those in our care – to show the same love, compassion, and respect for people that Jesus did. Pastoral care has been a key element of HammondCare’s relationship-based care for more than 90 years. It is an important way for us to champion the intrinsic value of each person.
Approach
Spirituality and spiritual care are at the heart of how we care for the whole person. Endorsed as being an essential part of quality care, spiritual care is delivered most directly through our Pastoral Care Coordinators and Pastoral Volunteers. They are trained to provide care and support to patients, residents and clients, and their support networks from a range of religious and cultural backgrounds. They work in partnership with the wider support team to ensure that spiritual and pastoral care is integrated into the care plans of all residents, patients and clients. HammondCare’s pastoral care service helps nurture the emotional and spiritual wellbeing of our clients, residents and patients, as well as their families, by helping them feel more connected and supported as they face health and ageing challenges. It may include religious services and activities for those seeking these.
HammondCare’s approach to spiritual care is:
- respectful
- gracious
- characterised by curiosity and listening
- for all faiths and none
- Christian in motivation.
At HammondCare, spiritual care includes:
- Tailored spiritual support based on individual client and residents needs and preferences. HammondCare addresses the spiritual and emotional needs of individuals in our care, regardless of their religious beliefs.
- Pastoral care and prayer, chapel services, spiritual reminiscence groups, and other group activities. Through these activities, our Pastoral Care Coordinatorsoffer the gift of time and listening, and often liaise with local faith representatives to provide specific faith ceremonies, rituals and conversations.
- Faith-based resources for people living with dementia, recognising that faith endures through every season of life, including for people living with dementia. The Faith for life suite of resources acknowledge the profound dignity of the person with dementia, their desire to express and explore faith while also recognising changing needs.[1]
[1] HammondCare (2022). Pastoral/Faith Resources